Knee Orthosis
Custom vs. Off-the-Shelf Knee Orthoses
Custom
- Better fit
- Decreased pistoning
- Increased rigidity
- Provides more control
Decision based on:
- Increased activity (competitive athlete)
- Decreased acitity (ADL’s)
- Patient anatomy
- Degree of instability
- Abnormal angulation
Knee Orthoses by Type
Knee Sleeve
- Simplest design
- Tube of stretch cotton or neoprene pulled lightly over the joint
- Minimal reduction or translatory and rotational motion
- No reduction of Ab/Adduction or Flexion/Extension
- Offers a “warming effect”
Stabilized Knee Sleeve/Knee Sleeve with Side joints
 Stabilized Knee Sleeves – varying degrees of rigidity
Stabilized Knee Sleeves – varying degrees of rigidity
Spiral Stays
- Slignt increase in translatory and rotational control
Hinges
- Uniaxial or polycentric
- With or without 180 degree stop
- Controls ab/adduction
**Polycentric more closely approximates anatomic knee motion and contributes to better stabilization of orthosis on wearers leg
Rigid Frame Knee Braces
Rigid Frame Orthoses
- Rigid framework of hinges and bands
- Pad, cuff, and strap design is based upon biomechanical deficit or patient
- Maximum control of ab/adduction or flexion/extension
- Roation difficult to control
- Extension stop at 10 degrees flexion helps
- Increased tissue coverage
- Increased friction material
- Bony lock
- Snugness
Knee Braces By Type of Need
Varus/Valgus Stabilizing Knee Braces
 Orthotic Requirements for Different Biomechanical Deficits
Orthotic Requirements for Different Biomechanical Deficits
I. Varus/Valgus Instability
- Commonly seen in Rheumatoid Arthritis, Osteoporosis, DJD
- Generalized joint destruction
- Bony erosions
- LCL/MCL laxity
- Genu Varum “bow-legs”
- Lateral lean of tibial plateau
- Disruption of lateral structures:
- lateral collateral
- biceps tendon
- iliotibial tract
- with or w/o medical meniscal involvement
- Genu Valgum “knock-knees”
- Medial lean of tibial plateau
- Disruption of medial structures
- medial collateral ligament
- PCL
- ACL
ACL or PCL Stabilizing Braces
II. Anterior / Posterior Instability
- Usually a result of trauma
- Rarely pure A-P instability
- Bony erosions
- ACL/PCL deficient
- Goals:
- Decrease abnormal motion
- Improve Function
**4-point force systems
III. Rotary Instability
- Commonly seen after severe multiligamentous trauma
- Usually involvement of med/lat collateral and ACL
- Ex. “unhappy triad” due to planting and turning
- Goals:
- Control tibial rotation about its longtitudinal axis
- difficult due to soft tissue of thigh
- Increase control by:
- limiting extension by approx. 10 (“screw home”)
- increase tissue coverage of cuff
- increase cuff friction
- rigid cuffs shaped to lock onto bony anatomy
- Control tibial rotation about its longtitudinal axis
IV. Hyperextension of the knees
- Ligament damage
- Capsular laxity
- Muscle weakness (quads, hamstrings)
- Commonly seen in patients with CVA, Post-Polio, CP
- Goals:
- Decrease destructive effects
- Improve function
- Correct alignment / Reduce deformity
**3-point force systems
PCL – Cti
V. 3 Custom Knee Orthosis – Seattle Systems


Premier – Townsend Design
Cti2 (custom), Cti2 Aspire (woman), Edge Aspire – Innovations Sports

Patellar Stabilizing Knee Braces
 VI. Patellar Instability
VI. Patellar Instability
- Recurrent subluxation or dislocation
- Pain
- Risk Factors:
- Excessive antiversion
- Increased Q angle (genuvalgum)
- Muscle imbalance (vastus lateralis overpull)
- Goals:
- Control pain
- Improve tracking
VII. Weakness
Quadriceps
- Knee buckling at heel strike
- Commonly seen in CVA patients
- Goal:
- Maintain extension through force systems
- Mostly treated with AFO or KAFO
Hamstrings
- Not usually managed orthotically, primary function in stance is to prevent hip flexion at heel strike
- Patient usually exhibits posterior trunk bending
Osteoarthritis Braces
 Osteoarthritis (OA), also called degenerative joint disease, is the break down of cartilage in the knee joint. As one grows older, the wear and tear of daily living and activity slowly wear out the joint. Knee trauma, such as broken bone, cartilage and/or supportive ligaments, can disrupt the integrity of the joint, leading to premature OA.
Osteoarthritis (OA), also called degenerative joint disease, is the break down of cartilage in the knee joint. As one grows older, the wear and tear of daily living and activity slowly wear out the joint. Knee trauma, such as broken bone, cartilage and/or supportive ligaments, can disrupt the integrity of the joint, leading to premature OA.
Symptoms can include a low grade ache and/or swelling, and become worse as the joint is used throughout the day.
OA is treated with knee braces as discussed above with medial/Lateral instability
Brace samples are as follows:

Post Op and ROM Braces
Generally prescribed post-operative or post-trauma. This type of brace is designed to help support the knee as well as limit the range of motion (ROM) to whatever angles the doctor specifies.

Dynamic ROM Braces
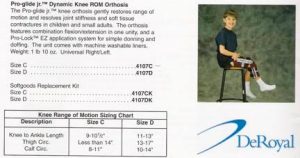
Munufacturers: dynasplint – rent only, ultraflex, Ortho innovations /Mackie DeRoyal / Pro-glide
Static-Progressive Stretch
Static progressive stretch (SPS) orthoses (braces) are used to restore lost range of motion to contracted joints through the biomechanical principle of stress relaxation. Soft tissues respond as a viscoelastic material. Soft tissues include tendons, ligaments, muscles, joint capsules, skin and fascia. As a viscoelastic material is stretched and then held at a constant length, the stress or tendency to rebound gradually declines. This decline in force is called stress relaxation. SPS used to stretch soft tissue uses a series of incremental changes in the joint position held constant over prescribed periods of time. Connective tissue responds favorably to this low-load prolonged stretch. This desired response allows the tissue to slowly adapt to the elongated length, resulting in permanent plastic deformation in the most time efficient manner.
Patient Application Instructions: Knee
1. Turn knobs (A) so the angle of the brace is the same as the leg. The leg should be in the most extended position.
2. The knee cap should be positioned between the two middle straps, with the brace on the front of the leg. Pull the straps (B) across the back of the leg and through the buckle. Straps should be secure and snug.
3. Turn the knobs together in the direction to straighten the knee until the patient experiences mild discomfort or a feeling of stretch. This feeling should reduce in less than 30 minutes. Follow prescribing physician’s instructions for length of wear, and specific knob adjustment.
THE MACKIE HINGE KNEE BRACE
 The Mackie Hinge Knee Brace was developed on the basis of our success with the Mackie Hinge Elbow Brace. The Mackie Hinge Knee Brace uses a unique rotating hinge mounted on a rigid, non-contact frame. This design offers simplicity of function, strong construction, and superior patient comfort. The Mackie hinge mechanism is engineered to allow for smooth and infinite positional settings. Because human physiology varies greatly from individual to individual, the hinge adjustability allows the patient to control how much force is applied to achieve the best result. For this patient-directed approach to be successful, patient tolerance and compliance is crucial. Static-Progressive Stretch is a proven concept for effective and permanent gain in range of motion.
The Mackie Hinge Knee Brace was developed on the basis of our success with the Mackie Hinge Elbow Brace. The Mackie Hinge Knee Brace uses a unique rotating hinge mounted on a rigid, non-contact frame. This design offers simplicity of function, strong construction, and superior patient comfort. The Mackie hinge mechanism is engineered to allow for smooth and infinite positional settings. Because human physiology varies greatly from individual to individual, the hinge adjustability allows the patient to control how much force is applied to achieve the best result. For this patient-directed approach to be successful, patient tolerance and compliance is crucial. Static-Progressive Stretch is a proven concept for effective and permanent gain in range of motion.
The Mackie Hinge Knee Brace also has the ability to be used in both flexion and extension. This can avoid the added expense of a second brace because many patients require stretch in both directions. It also helps reduce the risk that range of motion might be lost in the opposite direction. Patient Application Instructions are easy to understand. Physician prescribed Wearing Protocols allow the patient to incrementally stretch the joint to tolerance by turning the knobs to increase range of motion in either flexion or extension. The Mackie Hinge Knee Brace can be used with a variety of wearing protocols, that may be customized based on physician preference and patient need. Always follow your physicians instructions if they are different from our suggestions.
